An unexpected developmental hierarchy in an unusual disease
Share
Langerhans cell histiocytosis (LCH) is a rare disease affecting primarily young children. While LCH may heal by itself without treatment in some patients, others require intensive chemotherapy and suffer from long-term consequences, or may even succumb to the disease. The reasons for these differences in disease severity are poorly understood. In a new study published in Cancer Discovery, researchers from the St. Anna Children’s Cancer Research Institute (CCRI) and the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences revealed important insights into the cellular heterogeneity and molecular mechanisms underlying LCH.
Langerhans cell histiocytosis (LCH) is a very unusual disease: Often classified as a cancer because of uncontrolled cell growth in different parts of the body, it also has features of an autoimmune disease, as LCH lesions attract immune cells and show characteristic tissue inflammation. LCH is clinically variable and often difficult to diagnose. Skin involvement in babies with LCH can look like a nappy rash, whereas bone involvement can be mistaken as sarcoma in an X-ray picture. In its most aggressive form, LCH can present as leukaemia-like disease and lead to organ failure. These diverse manifestations and the enormous clinical heterogeneity of LCH continue to puzzle medical doctors and scientists around the world.
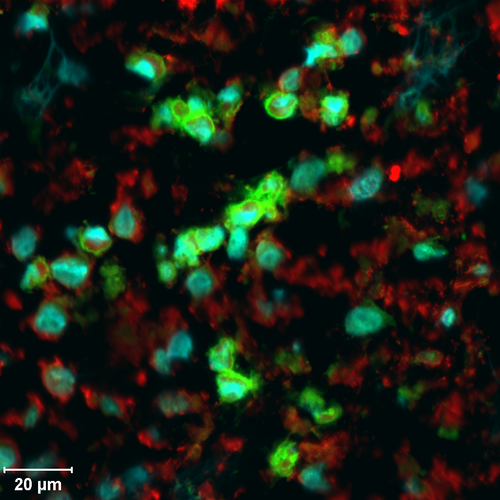
Studying LCH lesions under the microscope, Caroline Hutter – a paediatric oncologist at St. Anna Children’s Hospital, principal investigator at CCRI and co-lead investigator of this study – observed striking heterogeneity among LCH cells. To investigate this diversity in full molecular detail, she assembled an interdisciplinary team including experimental and computational researchers from CCRI and CeMM, as well as medical doctors from St. Anna Children’s Hospital and Vienna General Hospital. Her aim was to answer two fundamental questions: What are the mechanisms behind LCH, and how can we improve treatment of children affected by this disease?
Utilizing state-of-the-art technology in the laboratory of co-lead investigator Christoph Bock (CeMM), LCH lesions were analysed for their molecular composition at single-cell resolution. Spearheaded by one computational postdoc, Florian Halbritter (now at CCRI), and one wet-lab postdoc, Matthias Farlik (now at Medical University of Vienna), the team analysed the molecular profiles of LCH lesions and developed a comprehensive map of cellular heterogeneity in LCH.
In this molecular map of LCH, the team identified multiple LCH cell subtypes. One of these subtypes comprised actively dividing cells, which appear to give rise to the other LCH cell subtypes. In further experiments, the team unravelled the molecular pathways that are active in different branches of this unexpected developmental hierarchy, which corroborated an interplay of developmental, immunological, and oncogenic mechanisms in LCH.
The study is a significant step forward in the understanding of this enigmatic disease. In future, these finding may help devise better ways of distinguishing severe from less severe disease cases, and they may even open up new treatment possibilities.
The study "Epigenomics and Single-cell Sequencing Define a Developmental Hierarchy in Langerhans Cell Histiocytosis" is published ahead of print in Cancer Discovery on 25 July 2019. DOI: 10.1158/2159-8290.CD-19-0138.
Authors: Halbritter F*, Farlik M*, Schwentner R, Jug G, Fortelny N, Schnöller T, Pisa H, Schuster LC, Reinprecht A, Czech T, Gojo J, Holter W, Minkov M, Bauer W, Simonitsch-Klupp I, Bock C#, Hutter C#. * These authors contributed equally to this work; # CB and CH jointly directed the research.
Funding: The study was partly funded by the Austrian Science Fund, the German Research Foundation, the European Research Council, the Austrian Academy of Sciences, and the Histiocytosis Association.
The St. Anna Children's Cancer Research Institute (CCRI), founded in 1988, develops and optimizes diagnostic, prognostic, and therapeutic strategies for the treatment of children and adolescents with cancer by combining basic research with translational and clinical research. The focus is on the specific characteristics of childhood tumour diseases in order to provide young patients with the best possible and most innovative therapies. Around 120 scientists and students are involved in ongoing research projects at CCRI. Dedicated research groups in the fields of tumour genomics and epigenomics, immunology, molecular biology, cell biology, bioinformatics and clinical research are working together to harmonize scientific experimental findings with the clinical needs of physicians. Every year, about 250 children and adolescents in Austria are diagnosed with cancer. Thanks to interdisciplinary research work on an international level, 70 to 80 % of the children affected can already be cured.